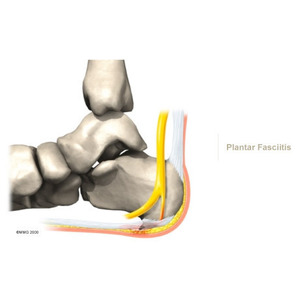
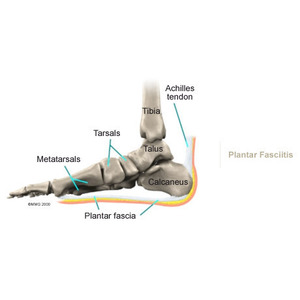
Nonsurgical management of plantar fasciitis is successful in 90 per cent of all cases. When you begin therapy at Physio Med, our physiotherapist will design exercises to improve flexibility in the calf muscles, Achilles' tendon, and the plantar fascia.
We will apply treatments to the painful area to help control pain and swelling. Examples include ultrasound, ice packs, and soft-tissue massage.
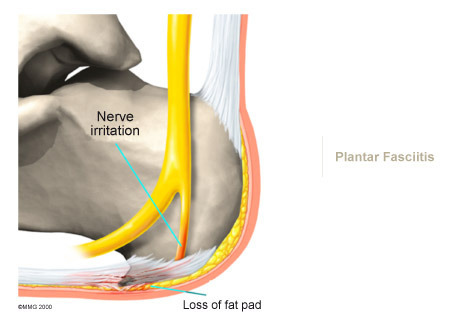
We may have a customized arch support, or orthotic, designed to support the arch of your foot and to help cushion your heel. Supporting the arch with a well fitted orthotic may help reduce pressure on the plantar fascia. Alternatively, we may recommend placing a special type of insert into the shoe, called a heel cup. This device can also reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration.
Your physiotherapist will also provide ideas for therapies that you can perform at home, such as doing your stretches for the calf muscles and the plantar fascia and using an ice bottle.
We find that many times it takes a combination of different approaches to get the best results for patients with plantar fasciitis. There isn't a one-size-fits-all plan. Some patients do best with a combination of heel padding, medications, and stretching. If this doesn't provide relief from symptoms within four to six weeks, then we may advise additional physiotherapy and orthotics.
Finding the right combination for you may take some time. Don't be discouraged if it takes a few weeks to a few months to find the right fit for you. Most of the time, the condition is self-limiting. This means it doesn't last forever but does get better with a little time and attention. But in some cases, it can take up to a full year or more for the problem to be resolved.
Doctors Review
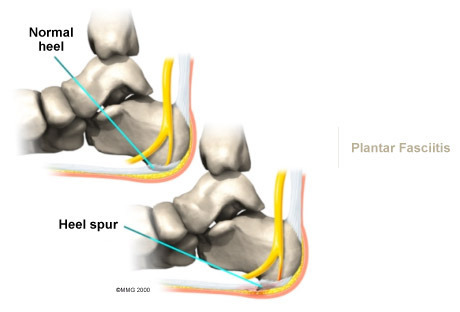
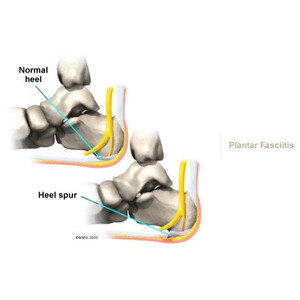
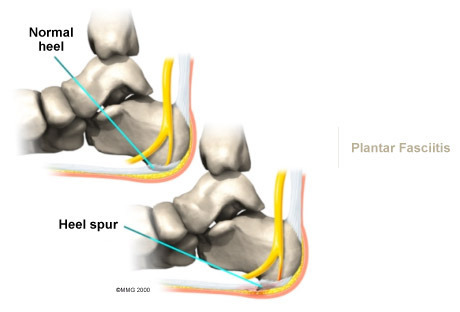
Your doctor may order an X-ray to rule out a stress fracture of the heel bone and to see if a bone spur is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasonographic exam may be favoured as it is quick, less expensive, and does not expose you to radiation.
A cortisone injection into the area of the fascia may be used. Studies show better results when ultrasound is used to improve the accuracy of needle placement. Cortisone should be used sparingly since it may cause rupture of the plantar fascia and fat pad degeneration and atrophy, making the problem worse.
Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Clinical trials are underway investigating the use of radiofrequency to treat plantar fasciitis. It is a simple, noninvasive form of treatment. It allows for rapid recovery and pain relief within seven to 10 days. The radio waves promote angiogenesis (formation of new blood vessels) in the area. Once again, increasing blood flow to the damaged tissue encourages a healing response.
Anti-inflammatory medications are sometimes used to decrease the inflammation in the fascia and reduce your pain. Studies show that just as many people get better with anti-inflammatories as those who don't have any improvement. Since these medications are rarely used alone, it's difficult to judge their true effectiveness.
Surgery
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas:
- remove the bone spur (if one is present)
- release the plantar fascia (plantar fasciotomy)
- release pressure on the small nerves in the area
Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision.
Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present that is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
Post-surgical Rehabilitation
Although recovery rates vary among patients, it generally takes several weeks before the tissues are well healed after surgery. The incision is protected with a bandage or dressing for about one week after surgery. You will probably use crutches briefly, and your physiotherapist can help you learn to properly use your crutches to avoid placing weight of your foot while it heals.
The stitches are generally removed in 10 to 14 days. However, if your surgeon used sutures that dissolve, you won't need to have the stitches taken out. You should be released to full activity in about six weeks.
Surgical release of the plantar fascia decreases stiffness in the arch. However, it can also lead to collapse of the longitudinal (lengthwise) arch of the foot. Releasing the fascia alters the biomechanics of the foot and may decrease stability of the foot arch. The result may be increased stress on the other plantar ligaments and bones. Fractures and instability have been reported in up to 40 per cent of patients who have a plantar fasciotomy.
Throughout your post-surgical recovery, our physiotherapist will note your progress and be watchful for the development of fractures and instability. When your recovery is well under way, regular visits to Physio Med will end. Although we will continue to be a resource, you will eventually be in charge of doing some therapeutic exercises as part of an ongoing home program.
Portions of this document copyright MMG, LLC.