Whenever possible, it is preferable to use treatments other than surgery. The first goal of these nonsurgical treatments is to ease your pain and other symptoms.
Nonsurgical treatments ease the symptoms in your neck and address the problem directly to resolve the underlying issue/s. At Physio Med, if a Physiotherapy program is appropriate one will be prescribed; and although each patient's recovery time varies, our treatments are designed to help ease pain and to improve mobility, strength, posture, and function.
Your Physiotherapist in Leeds may also advise you to intermittently place a hot or cold pack on your neck, or you may be shown how to do a contrast treatment. Contrast treatments involve switching between a cold pack and a hot pack.
At Physio Med, we will work with you to improve your neck movement and strength. We will also encourage healthy body alignment and posture. These steps are designed to slow the degeneration process and enable you to get back to your normal activities.
When your Physiotherapy programme is nearly completed, we may provide you with exercises to do at home on a regular basis to help control your symptoms and protect your neck in the years ahead.
Post-surgical Rehabilitation
Rehabilitation after surgery is much more complex. Some patients leave the hospital shortly after surgery, but some surgeries require patients to stay in the hospital for a few days.
A Physiotherapist will often visit you in your hospital room soon after surgery. These initial in-hospital treatment sessions help our patients learn to move and do routine activities without putting extra strain on the neck.
Many surgical patients need Physiotherapy outside of the hospital as well. Although the time required for rehabilitation varies for each patient. Our Physiotherapy treatments are designed to calm pain and muscle spasm, teach patients to move safely, and help patients develop strength and mobility.
As our Physiotherapy sessions come to an end, your Physio Med Physiotherapist may help you get back to work. We can do a work assessment to ensure you can do your job safely. Some patients may need to modify their work or other activities to avoid future problems.
At Physio Med, our goal is to help you keep your pain under control, improve your range of motion, and maximise strength and control in your neck. When your recovery is well under way, regular visits to our clinic will end. We will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home programme.
Other Tests and Treatments
Electromyogram
An electromyogram (EMG) is a special test used to determine if there are problems with any of the nerves going to the upper limbs. EMGs are usually done to determine whether the nerve roots have been pinched by a herniated disc. During the test, small needles are placed into certain muscles that are supplied by each nerve root. If there has been a change in the function of the nerve, the muscle will send off different types of electrical signals. The EMG test reads these signals and can help determine which nerve root is involved.
Laboratory Tests
Not all causes of neck pain are from degenerative conditions. Doctors use blood tests to identify other conditions, such as arthritis or infection. Other tests may be needed to rule out problems that do not involve the spine.
Medications
Many different types of medications are typically prescribed to help gain control of the symptoms of neck pain. There is no medication that will cure neck pain. Your Doctor may prescribe medications to ease pain, fight inflammation, and to help you get a better night's sleep.
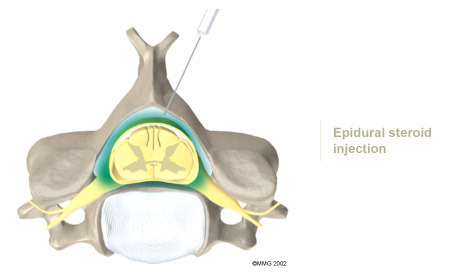
Injections
Spinal injections are used for both treatment and diagnostic purposes. There are several different types of spinal injections that your Doctor may suggest. These injections usually use a mixture of an anesthetic and some type of cortisone preparation. The anaesthetic is a medication that numbs the area where it is injected. If the injection takes away your pain immediately, this gives your Doctor important information suggesting that the injected area is indeed the source of your pain. The cortisone decreases inflammation and can reduce the pain from an inflamed nerve or joint for a prolonged period of time.
Some injections are more difficult to perform and require the use of a fluoroscope. A fluoroscope is a special type of X-ray that allows the Doctor to see an X-ray picture continuously on a TV screen. The fluoroscope is used to guide the needle into the correct place before the injection is given.
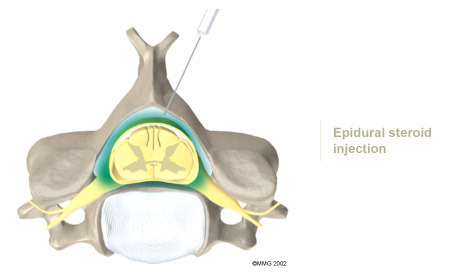
Epidural Steroid Injection: Neck pain or pain that spreads down the arm may require treatment with an epidural steroid injection (ESI). In an ESI, the medication mixture is injected into the epidural space around the nerve roots. Generally, an ESI is given only when other non operative treatments aren't working. ESIs are not always successful in relieving pain. If they do work, they may only provide temporary relief.
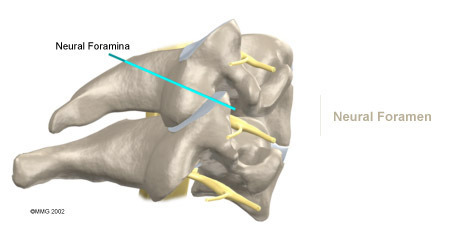
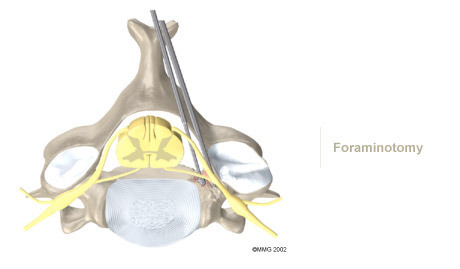
Selective Nerve Root Injection: Another type of injection to place steroid medication around a specific inflamed nerve root is called a selective nerve root injection. The fluoroscope is used to guide a needle directly to the painful spinal nerve. The nerve root is then bathed with the medication. Some doctors believe this procedure gets more medication to the painful spot. In difficult cases, the selective nerve root injection can also help surgeons decide which nerve root is causing the problem before surgery is planned.
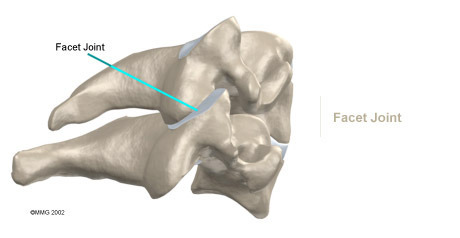
Facet Joint Injection: When the problem is thought to be in the facet joints, an injection into one or more facet joints can help determine which joints are causing the problem and ease the pain as well. The fluoroscope is used to guide a needle directly into the facet joint. The facet joint is then filled with medication mixture. If the injection immediately eases the pain, it helps confirm that the facet joint is a source of pain. The steroid medication will reduce the inflammation in the joint over a period of days and may reduce or eliminate your neck pain.
Trigger Point Injections: Injections of anaesthetic medications mixed with a cortisone medication are sometimes given in the muscles, ligaments, or other soft tissues near the spine. These injections are called trigger point injections. These injections can help relieve neck pain and ease muscle spasm and tender points in the neck muscles
Portions of this document copyright MMG, LLC.